Telehealth has skyrocketed under the pandemic worldwide. Currently, 46% of visits are delivered online, and 76% of consumers are interested in telehealth, as McKinsey experts state. Compared with 2019, when burdened with legal regulations, it was reaching about 11% of usage among US patients. We present a detailed analysis of the most promising medical specialties integrating telehealth in the US. See what healthcare providers have implemented already and what changes are coming.
Telehealth is likely to stay a growing trend in the post-pandemic era. Adopting telemedicine practices was reluctant before 2020. But now, it promises that $250 billion in the US could be potentially virtualized. To begin with, let us define how much “health” is in telehealth.
Per WHO (World Health Organization), telehealth is the “delivery of health care services, where patients and providers are separated by distance.” Telehealth leverages ICT networks to transmit information on diagnosis, treatment, research, evaluation, diseases, injuries, and education.
Meanwhile, one can often see the narrower term — telemedicine. It refers to the medical services provided by several electronic technologies, focusing primarily on monitoring and diagnosis. Telemedicine is different from telehealth, which breaks down into long-distance patient care, admission, monitoring, advice, reminders, and even intervention.
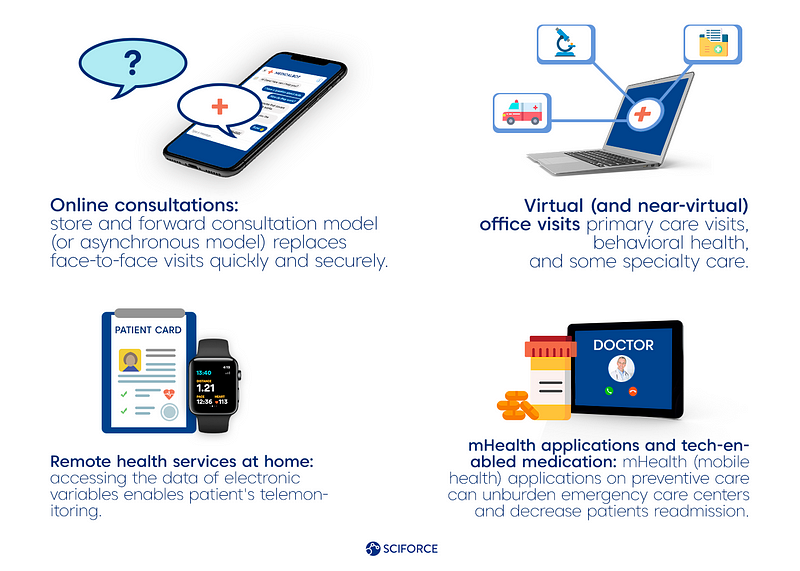
Practically, telehealth encompasses the following services:
The pandemic’s stroke resulted in the rise of remote monitoring and care management for internists and family physicians (FPs) too. Depending on the specialty, there is a variance in using video visits and asynchronous evaluation of data and images, but the subspecialists and general internists prefer the latter.

Having a lot in common with internists but focusing on different fields, FPs are reported to represent primary care providers’ biggest platform in the US. Hence, it potentially can integrate with many telemedicine practices. Recent surveys state that patients are provided with remote blood pressure monitoring, and parents are satisfied with acute pediatric telehealth services due to their convenience during the quarantine.
In light of further developments, healthcare providers will resolve the questions of the store and forward vs. live video calls, eliminating the barriers in usage for patients and dealing with upcoming changes in the regulation of telehealth.
Radiology has always been the keenest early adopter of telehealth. Per the nationally representative survey of the American Medical Association (AMA), radiology hit the top of the list with 39.5% usage for patient interaction among other specialties in 2018.
In light of telemedicine gaining momentum in 2021, teleradiology “will become more of a standard way of practicing medicine,” says Dr. Kim, CTO at Texas Radiology Associates (TRA). Offsite radiologists provide medical facilities with benefits like cost reduction, higher efficiency, access to rural areas, sharing subspecialty expertise and second opinions, etc.
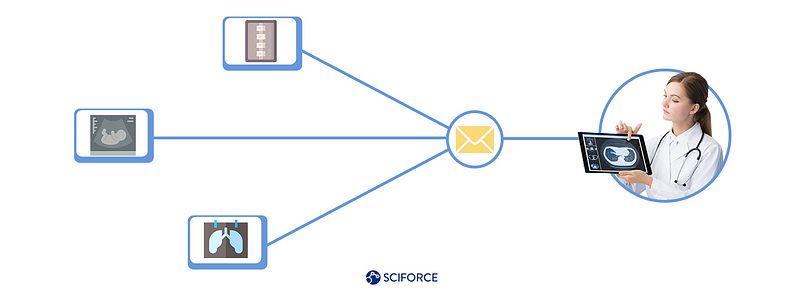
Simply put, teleradiology is easily applicable to the following radiological image processing:
On the other hand, as the industry learns how to tackle the pandemic, the question of keeping a sound balance between offsite and onsite radiologists arises. For example, remote reading is not applicable for lumbar puncture (LP) or abscess drainage, as these techniques require imaging guidance. Thus, telecommuting is not an option for interventional radiologists and radiology technologists anyway.
Telepsychiatry is likely to remain more popular compared to the pre-pandemic baselines, as researchers state. Per the Agency for Healthcare Research and Quality, one in eight emergency room visits in the US is linked to substance use or mental health. Simultaneously, not every emergency center can provide healthcare to a person with a severe mental disorder or has a devoted specialist on staff.

Moreover, psychiatrists have successfully applied telemedicine practices under the COVID-19. For example, telepsychiatry reached 48.3% of overall telemedicine visits among nine surveyed California clinics in September 2020. Healthcare providers state the following perks:
Per the American Psychiatric Association, telepsychiatry is "equivalent to in-person care in diagnostic accuracy, treatment effectiveness, quality of care, and patient satisfaction." At the same time, patient privacy and confidentiality are equivalent to in-person care as a result of the changes regarding HIPAA compliance during the pandemic in the US.
As a result, further questions for post-pandemic telepsychiatry refer to the scaling of telemedical practices, changing the way of gathering and analyzing healthcare data, and adapting new hybrid models for healthcare providing.
Even though researchers in telemedical neurology were published in the early 2000s, it gets pandemic-induced acceleration now. It dramatically increased during the first weeks of the pandemic — a 2,000% surge in the Mayo Clinic, Arizona stands as an example. Hence, it launches a broad discussion on the changes in the specialty.

Practically, teleneurology is applicable for the following cases:
Meanwhile, while safety is the main reason for increasing the demand for teleneurology, it still has some disadvantages. As healthcare providers state, the virtual exam can be equivalent to the physical when it goes about the gaze, vision, strength, speech, memory, mental function, sensation, balance, and coordination.
However it is hard to assess muscle tone, visual fields, subtle eye movements, and comprehensive sensory examination. In such cases, patients need the help of another person at their side. We consider that the hybrid approach is also about the future of teleneurology.
Like other medical specialties integrating telehealth, dermatology encounters its perks and perils. Teledermatology is well-suited to deliver healthcare during the pandemic, as high-resolution images sent from a primary care provider are sufficient for diagnosis. Moreover, skin condition examination can prevent various internal diseases, like liver diseases, cancers, blood clotting disorders, autoimmunity, teledermatology.

On the other hand, some procedures (e.g., biopsies, surgeries), advanced treatments, and complete physical examinations are provided in the clinics only. Leveraging intelligent policies and regulations, care providers can optimize their work and benefit from hybrid approaches.
As researchers state, the advantages of teledermatology include:
One of the surveys shows that the implementation of teledermatology workflow can result in a 9% increase in skin cancer identification with 39% fewer in-person dermatology visits. It is beneficial for quarantining patients.
Radiology, psychiatry, neurology, dermatology, internal medicine, and family care successfully integrate telehealth practices under the pandemic. They are leveraging the best practices developed and lessons learned too.
Hence, we consider the hybrid approaches in delivering efficient healthcare to become more popular while tackling the pandemic and applying the AI techniques more widely. We will tell how the industry can quickly scale telemedicine practices and boost its capabilities using AI in our next blog in this series.