AI is transforming cancer care in incredible ways, and understanding how its success is measured is key to assessing its impact. In this article, we’ll start with a quick, straightforward explanation of key AI metrics like AUC and Dice scores.
Once that foundation is set, we’ll explore real-world research showing how AI is advancing early cancer detection, improving diagnoses, personalizing treatments, and even speeding up drug discovery. These examples demonstrate how AI is making cancer care more precise, effective, and life-saving.
In our previous article, we explored new AI technologies like radiomics and tumor evolution models, paving the way for personalized oncology. This one shifts focus to real-world research outcomes in different areas of oncology.
AI is revolutionizing cancer care, but how do we measure its success? Below is a simple guide to the key metrics and methods used to evaluate AI’s performance.
These metrics help assess how well an AI model performs tasks like detecting cancer or predicting outcomes:
These metrics show how effectively the AI detects or excludes specific conditions:
Validation methods ensure the AI works well in different settings and with new data:
This framework ensures that AI technologies in oncology are not only accurate but also practical and adaptable for real-world use.
By integrating advanced technologies like deep learning, radiomics, and predictive analytics, AI is enabling earlier interventions, more accurate diagnoses, and personalized care strategies. To create this article, our medical team gathered and analyzed some of the most impactful and recent research across key areas of oncology.
Artificial intelligence is revolutionizing the early detection of cancer, offering innovative ways to identify high-risk patients and diagnose cancers using non-invasive techniques.
Predicting High-Risk Patients
AI is transforming cancer care by enabling earlier detection, especially for aggressive cancers like pancreatic cancer. A 2023 study in Nature Medicine introduced CancerRiskNet, a machine learning model analyzing over 9 million patient records to predict high-risk individuals up to three years earlier than traditional methods. It achieved an AUROC of 0.88 in Danish data and improved US performance to 0.78 after retraining. Early identification through this model offers a vital chance to enhance survival rates for cancer where late-stage diagnosis often limits outcomes.
Cancer Diagnosing with Liquid Biopsies Shivashankar et al. (2024) created an AI-based method to study chromatin organization in PBMCs from liquid biopsies. The tool achieved 77% accuracy in distinguishing healthy individuals from various cancers patients and 78% in identifying glioma, meningioma, and head and neck tumors. It also monitored proton therapy effects by detecting changes like reduced nuclear size and DNA damage, providing insights into treatment response and tumor behavior.
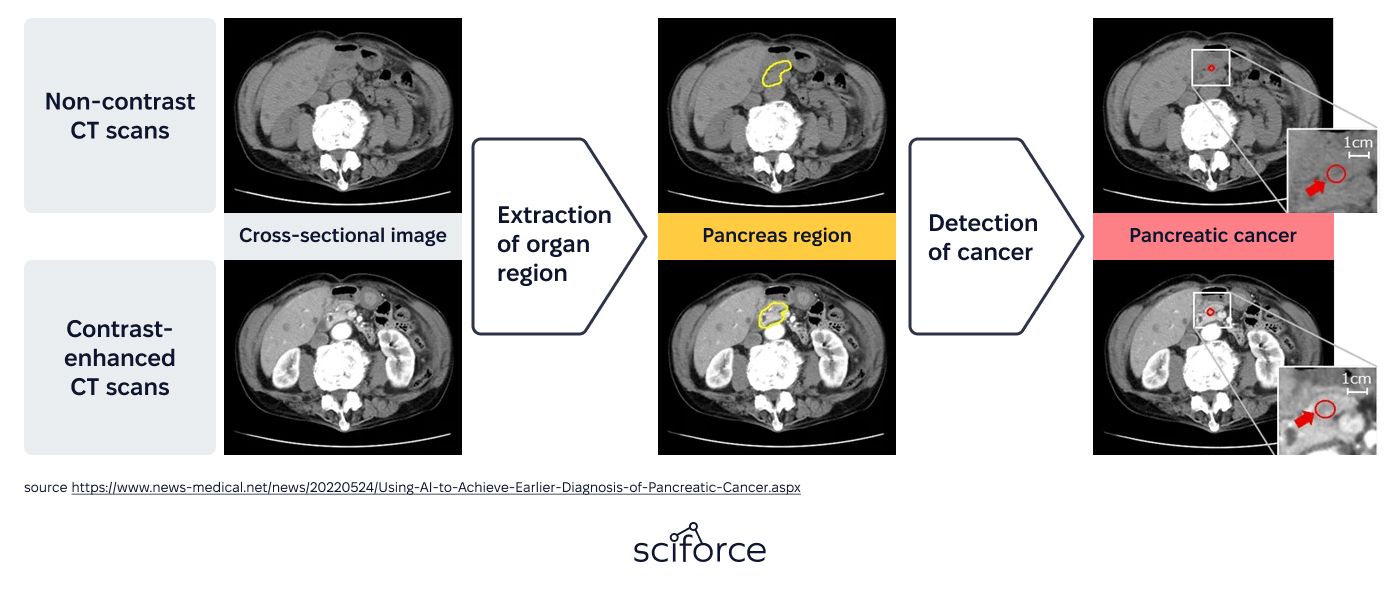
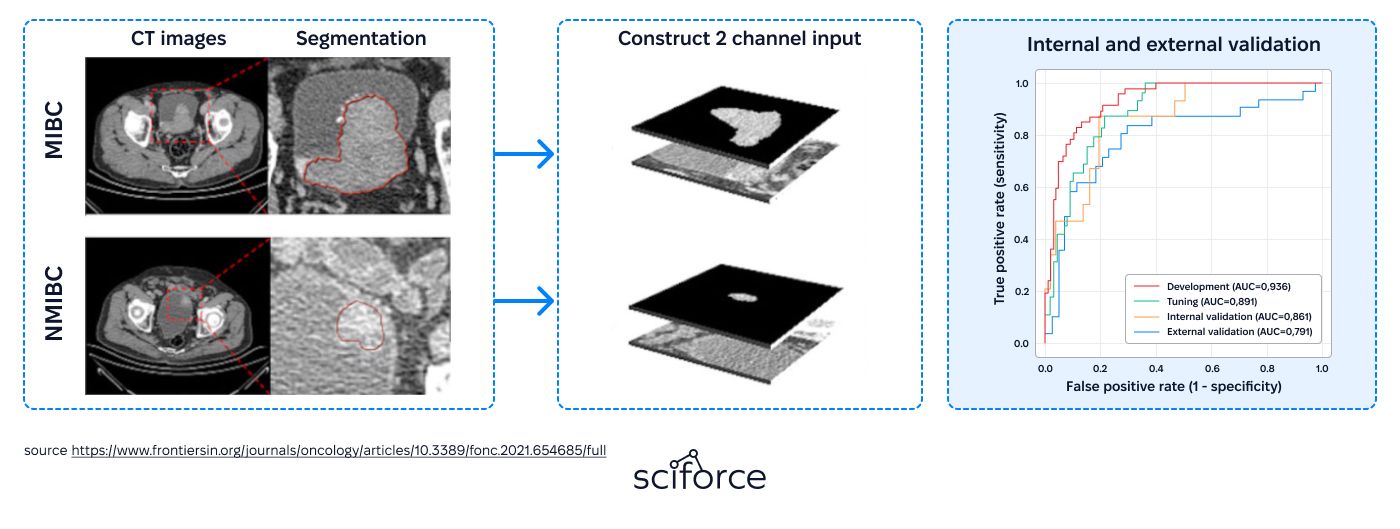
AI has made significant strides in medical imaging, particularly in tumor detection and classification using technologies like CT, MRI, and PET scans. These advancements improve diagnostic consistency and reduce variability, providing radiologists with powerful tools to enhance care.
A study published in Frontiers in Oncology (Zhang et al., 2021) presented a deep learning model called FGP-Net that predicts whether bladder cancer has invaded muscle tissue using enhanced CT images. The model showed strong performance, achieving AUC scores of 0.861 during internal testing and 0.791 in external validation, outperforming radiologists in both accuracy and consistency. This advancement improves preoperative evaluations and helps doctors plan more effective treatments.
A study by Jiménez Gaona et al. (2024) highlights how AI is advancing breast cancer diagnosis. By leveraging tools like convolutional neural networks (CNNs) and generative adversarial networks (GANs), the researchers analyzed medical images using datasets like CBIS-DDSM and BUSI, achieving a segmentation AUC of 0.88.
To overcome limited data, they used GANs to generate synthetic images, improving breast lesion detection and classification. This research demonstrates AI's potential to make breast cancer diagnosis faster and more accurate, benefiting patients worldwide.
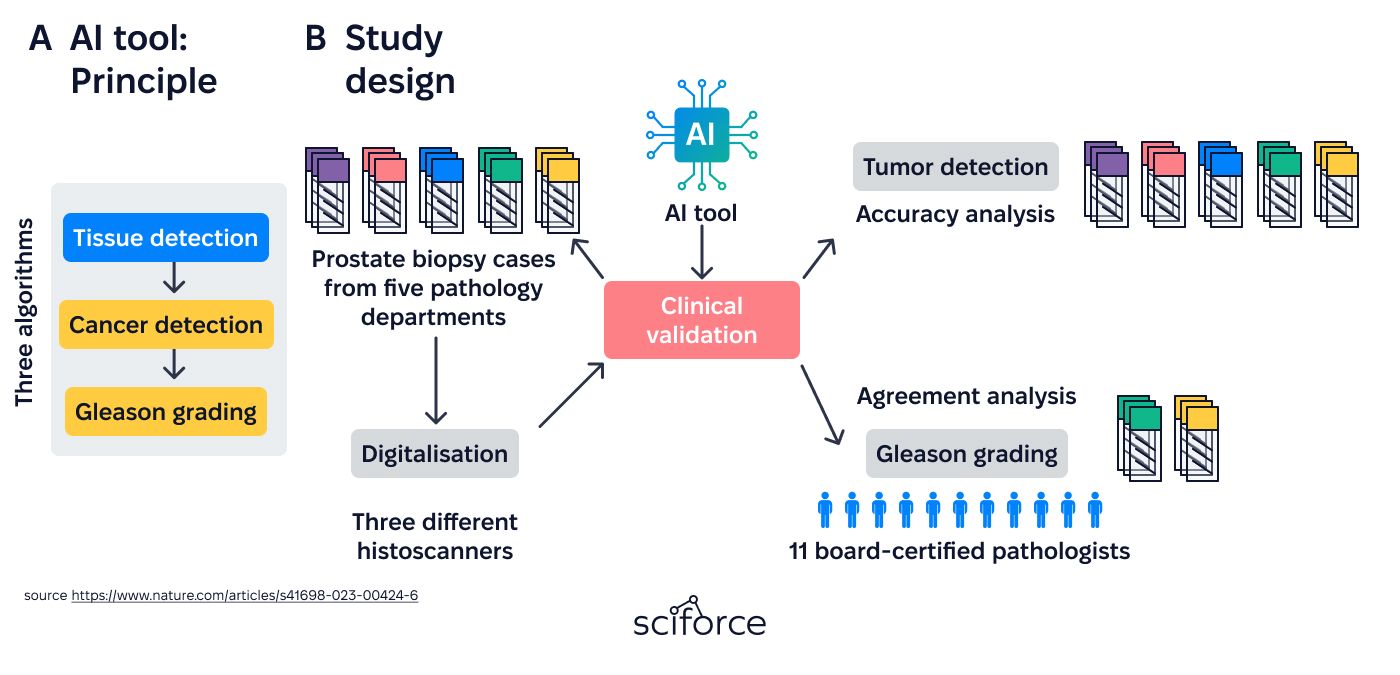
AI is revolutionizing digital pathology by streamlining complex tasks like detecting tumors in prostate biopsy samples.
A study by Tolkach et al. (2023) evaluated an AI tool for identifying prostate cancer and assigning Gleason grades, which measure cancer aggressiveness. Analyzing over 5,900 biopsy slides from five pathology centers, the tool achieved 97.1–100% sensitivity and 87.5–97.6% specificity.
The AI performed comparably to experienced pathologists, with a kappa score of 0.77, highlighting its ability to deliver consistent, expert-level evaluations while reducing variability in interpretation.
AI is transforming cancer treatment by delivering personalized solutions. By analyzing genetic and clinical data, AI identifies unique tumor markers, enabling precise therapies that target cancer cells while minimizing side effects.
AI is used in cancer treatment by identifying unique genetic or protein signals in tumors that act like fingerprints, guiding doctors to tailor treatments that precisely target only cancer cells.
Chen et al. (2020) developed a deep learning model using H&E-stained histopathology images to analyze liver tissue. Based on the **Inception V3 **neural network, it achieved 96% accuracy in distinguishing benign from malignant tissues, 89.6% for tumor differentiation, and AUCs of 0.71–0.89 for genetic mutations, enabling faster, personalized cancer diagnosis and treatment.
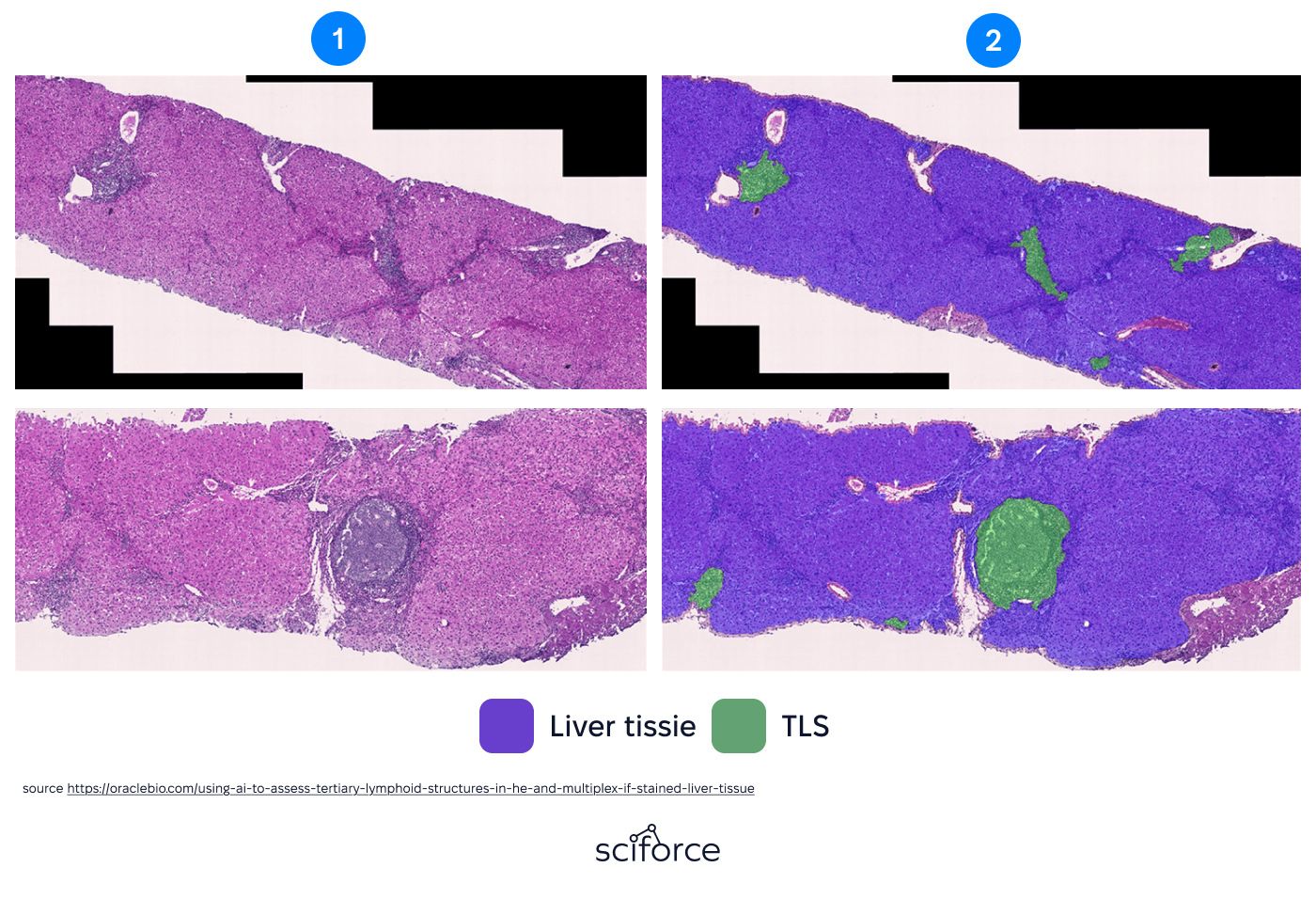
Some tumors have structures called tertiary lymphoid structures (TLSs), clusters of immune cells that signal the body’s response to cancer. Their presence often predicts better outcomes with immunotherapy, which strengthens the immune system to fight cancer.
Chen et al. (2024) developed an AI tool to identify TLSs in H&E-stained tissue samples, achieving Dice scores of 0.91 (internal) and 0.866 (external). Higher TLS levels correlated with stronger immune activity and better cancer responses. Incorporating TLS measurements into staging systems improved survival predictions, outperforming traditional methods in 10 of 15 cancer types.
AI helps doctors to predict how a cancer will respond to treatment before it even begins. AI can forecast treatment outcomes, track tumor changes in real time, and adjust therapies as your body responds. Here’s how it works:
Not every patient responds the same way to cancer treatment. AI dives deep into patient data – like tumor images, genetic profiles, and lab results – to figure out what will work best for each individual.
A study by Salgado and AbdulJabbar (2023) in The Lancet examined how tumor-infiltrating lymphocytes (TILs) – immune cells found in and around tumors – can serve as biomarkers in melanoma. Using imaging and advanced deep learning techniques, the researchers analyzed 321 primary and 191 metastatic melanoma samples to create an electronic TIL (eTIL) scoring system.
The eTIL score effectively predicted metastasis risk in primary melanoma and response to anti-PD-1 immunotherapy in metastatic cases. Patients with eTIL scores above 16.6% had better outcomes, including lower metastasis risk and improved treatment success, providing a valuable tool for guiding care.
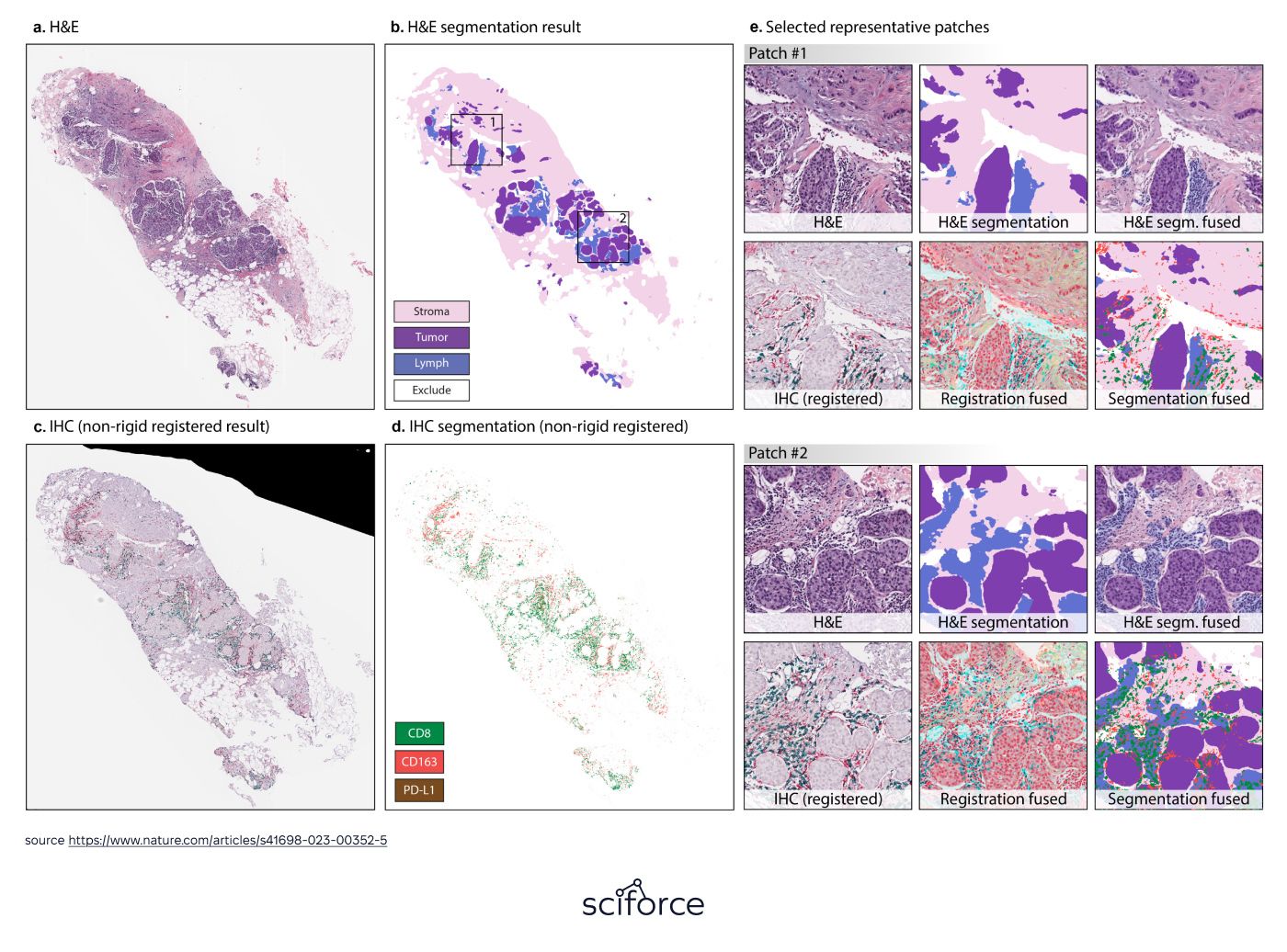
A Nature Cancer by Zhi Huang study showed how AI predicts breast cancer patient responses to neoadjuvant chemotherapy (NAC). Using histopathology and immunohistochemistry (IHC) images, researchers developed a model with the IMPRESS pipeline and LASSO regression, achieving AUCs of 0.8975 for HER2-positive and 0.7674 for triple-negative breast cancer. This approach outperformed traditional methods, enabling more tailored treatments.
What if doctors could watch how a tumor reacts to treatment in real-time? With AI, they can. These smart tools track tumor changes, helping doctors fine-tune therapies on the go.
A recent study in Cancers highlighted how AI improves predictions for nasopharyngeal carcinoma (NPC), a cancer affecting the nasopharynx, the uppermost part of the throat. Researchers analyzed 385 H&E-stained tissue samples, focusing on tumor-infiltrating lymphocytes (TILs), immune cells near tumors that provide critical prognostic information.
Using deep learning models like HoverNet and MorphResNet, the AI calculated TIL scores to group patients by high- and low-recurrence risk. With 92.1% accuracy, the study found that higher TIL scores were associated with a lower risk of cancer recurrence, offering valuable insights for personalized treatment planning.
Cancer is sneaky – it evolves as it’s being treated. AI-powered adaptive treatment plans ensure therapies stay effective, even as the disease changes.
A study by Feng et al. (2023) in Cancers examined how AI can enhance adaptive radiotherapy for breast cancer. Researchers tested the Ethos AI-based segmentation tool, which identifies key structures like breast tissue, heart, lungs, and lymph nodes from CBCT images. The tool showed high precision, with over 98% of structures needing minimal corrections, closely matching results from manual contouring.
Creating new cancer drugs has traditionally been a slow, expensive process, often taking years to develop a single treatment. AI is flipping the script by acting as a digital detective, looking through mountains of data in seconds to uncover potential life-savers.
AI is revolutionizing how we identify potential cancer drugs by predicting how molecules interact with cancer cells. This dramatically cuts down the time and cost of finding promising candidates. Some exciting results include:
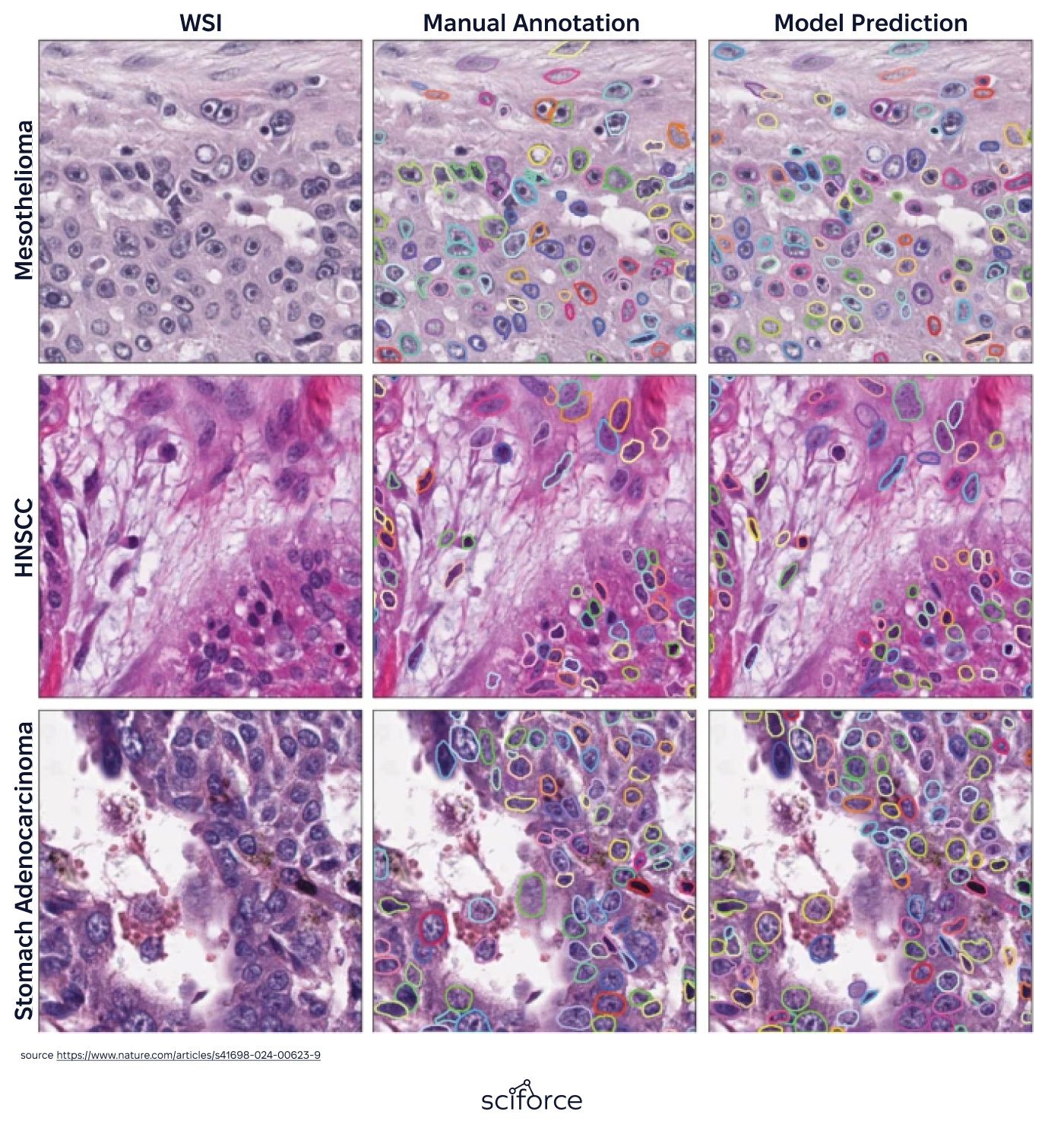
Abel et al. (2024), in a study published in Precision Oncology, created an AI-powered tool for digital pathology. The tool, based on a deep learning model similar to Mask-RCNN, analyzed H&E-stained tissue slides from breast, lung, and prostate cancers. It focused on identifying and segmenting cell nuclei while examining features like their shape, size, and texture.
The model showed strong performance, achieving a Dice score of 0.818. It also revealed important links between the appearance of cell nuclei – such as shape and size – and genetic factors like aneuploidy (abnormal chromosome numbers), which play a role in cancer progression.
AI isn’t just about finding drugs – it’s also transforming how clinical trials are conducted. Matching the right patient to the right trial or predicting outcomes has never been easier:
Zhang et al. (2024), in Frontiers in Oncology, developed AI models to predict the spread of breast cancer using blood tests, ultrasound scans, and biopsy data from two medical centers. They tested two methods: **Logistic Regression (LR) **and LightGBM. LightGBM performed better, with AUC scores of 0.971 during training, 0.861 in internal testing, and 0.890 in external testing. These results highlight LightGBM’s potential to predict early metastasis and support better treatment planning for breast cancer patients.
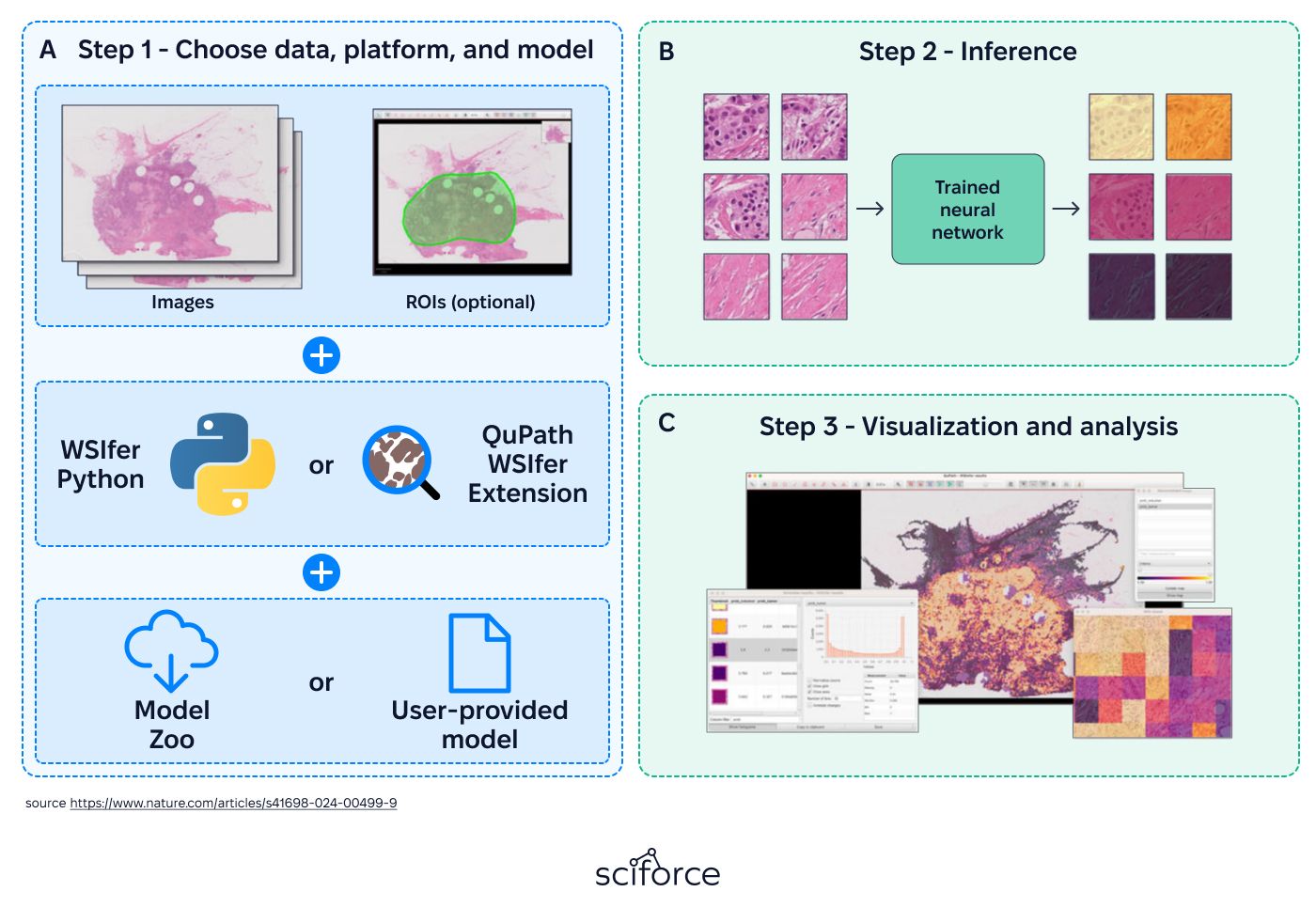
Kaczmarzyk et al. (2024), in NPJ Precision Oncology, introduced WSInfer, an open-source tool designed to simplify the use of deep learning models in digital pathology. Integrated with QuPath software, WSInfer helps classify tissue regions in whole slide images (WSIs) for diagnosing, predicting outcomes, and planning treatments in cancer care. It features a "Model Zoo" with pre-trained AI models for breast, colorectal, and lung cancers and enables researchers to map and analyze tissue characteristics effectively.
The research in this article highlights how AI improves diagnostic accuracy, predicts treatment responses, and accelerates drug discovery. Innovations like CancerRiskNet, WSInfer, adaptive therapies, and liquid biopsy technologies represent major advances in oncology.
However, challenges remain. Ensuring accessibility, improving data quality, and addressing disparities in adoption are critical steps to maximize AI’s potential in oncology. At SciForce, we deliver AI-driven healthcare solutions, from integrating diverse datasets to building predictive oncology models.
Contact us to discover how our expertise can advance smarter cancer care.