The client is a startup operating in the intersection of FinTech and Healthcare sectors, focusing on insurance claims management. They are addressing the issue of claim denials, a significant challenge within the U.S. healthcare system. Our client’s goal is to transform the current claim-handling process helping hospitals and medical practices to reduce financial losses and administrative burdens:
The goal of the product is to reduce the rate of claim denials and optimize the efficiency of claim processing, mitigating financial losses and administrative burdens.
The U.S. healthcare system faces a significant challenge with many insurance claims being denied. This issue leads to financial losses for hospitals and healthcare providers, as they often have to navigate through lengthy and complicated processes to get these claims approved:
High Rate of Claim Denials
The institutions face a large volume of denied claims, leading to revenue losses and increased administrative work.
Complex Claim Processing
The complexity of insurance policies and claim processing requires significant time and resources, often overwhelming the staff with additional paperwork.
Lack of Efficient Management Tools
Healthcare institutions often lack specialized tools to effectively predict and prevent claim denials, leading to reactive rather than proactive management.
Our solution combines automated claim assessment, AI-integrated streamlined processing, and predictive analytics to transform the challenges of high claim denials and complex processing in healthcare. The AI model we've developed not only automates and simplifies claim assessments but also anticipates potential denials, enabling proactive management.
The project's goal is to develop an AI model to assess and lower the risk of insurance claim denials. It features two key components: the CodeTerm, which processes and structures claim data, and the HealthClaim RejectionGuard, which focused on predicting claim outcomes to improve efficiency.
- Automated Claim Assessment:
To address the high rate of claim denials, we've developed an AI model that automates the assessment of claims, identifying potential denials early in the process. This helps in proactive management and reduction of denials.
- Streamlined Processing through AI Integration:
Our solution simplifies the complex claim processing workflow. By integrating advanced AI algorithms, we're able to process claims more efficiently, freeing up valuable time and resources for the hospital staff.
- Predictive Analytics for Prevention:
To overcome the lack of efficient management tools, our product includes predictive analytics features. This allows institutions to anticipate possible claim denials and take preventive measures, shifting from a reactive to a proactive approach in claim management.
Each of these solutions directly addresses the specific challenges faced by our target audience, offering a comprehensive and efficient approach to managing insurance claims in the healthcare sector.
Conceptualization
The initial stage involved brainstorming and conceptualizing a solution to tackle high claim denials in healthcare. The goal was to design and integrate an automated claim assessment, AI-driven streamlined processing, and predictive analytics to address the issue of a high number of claim denials in healthcare.
AI Model Development
We developed a model that not only automates claim assessments but can predict potential denial. The goal is to enable proactive, not reactive claims processing.
Testing and Refinement
Throughout the project, we conducted a large number of tests to enable accurate performance of the AI model. Based on test results, we enhanced the model's effectiveness in assessing the claims and predicting denials.
Data Quality and Integration
Challenge: Dealing with inconsistent or incomplete data from various sources. Solution: Implemented data cleansing and integration processes, with the development of data validation mechanisms. Collaborated closely with data providers to enhance data quality.
Model Accuracy and Interpretability
Challenge: Improving the AI model's accuracy in claim denial predictions and ensuring its interpretability Solution: Continuously trained and fine-tuned the model using diverse datasets. Adopted explainable AI techniques to improve model interpretability.
Regulatory Compliance
Challenge: Adhering to the complex healthcare regulations and compliance standards. Solution: Maintained up-to-date knowledge of healthcare regulations, integrating compliance checks and conducting regular audits for sustained compliance.
Scalability
Challenge: Ensuring the solution's capacity to handle increasing claim volumes. Solution: Designed the system for scalability, employing cloud infrastructure and performance-optimized code. Continually assessed and upgraded infrastructure to meet growing needs.
Privacy and Security
Challenge: Safeguarding the security and privacy of sensitive healthcare data. Solution: Implemented stringent security measures like encryption and access controls, aligning with healthcare data protection standards.
Technical Highlights
Our project's tech stack is robust and advanced, centered around Python 3 and SQL with AWS Redshift for effective database management. Key AI technologies include Random Forest and Extreme Gradient Boosting for predictive modeling, complemented by sophisticated Computer Vision techniques like OCR.
We leverage numpy and pandas for data analysis, with visualization through Matplotlib and seaborn. The machine learning framework is powered by sci-kit-learn and TensorFlow, while Flask facilitates our web framework needs. Docker is used for efficient containerization, ensuring scalability and streamlined deployment.
This model consists of two essential components: the CodeTerm streamlining data processing, and the HealthClaim RejectionGuard focusing on predictive analytics for claim outcomes.
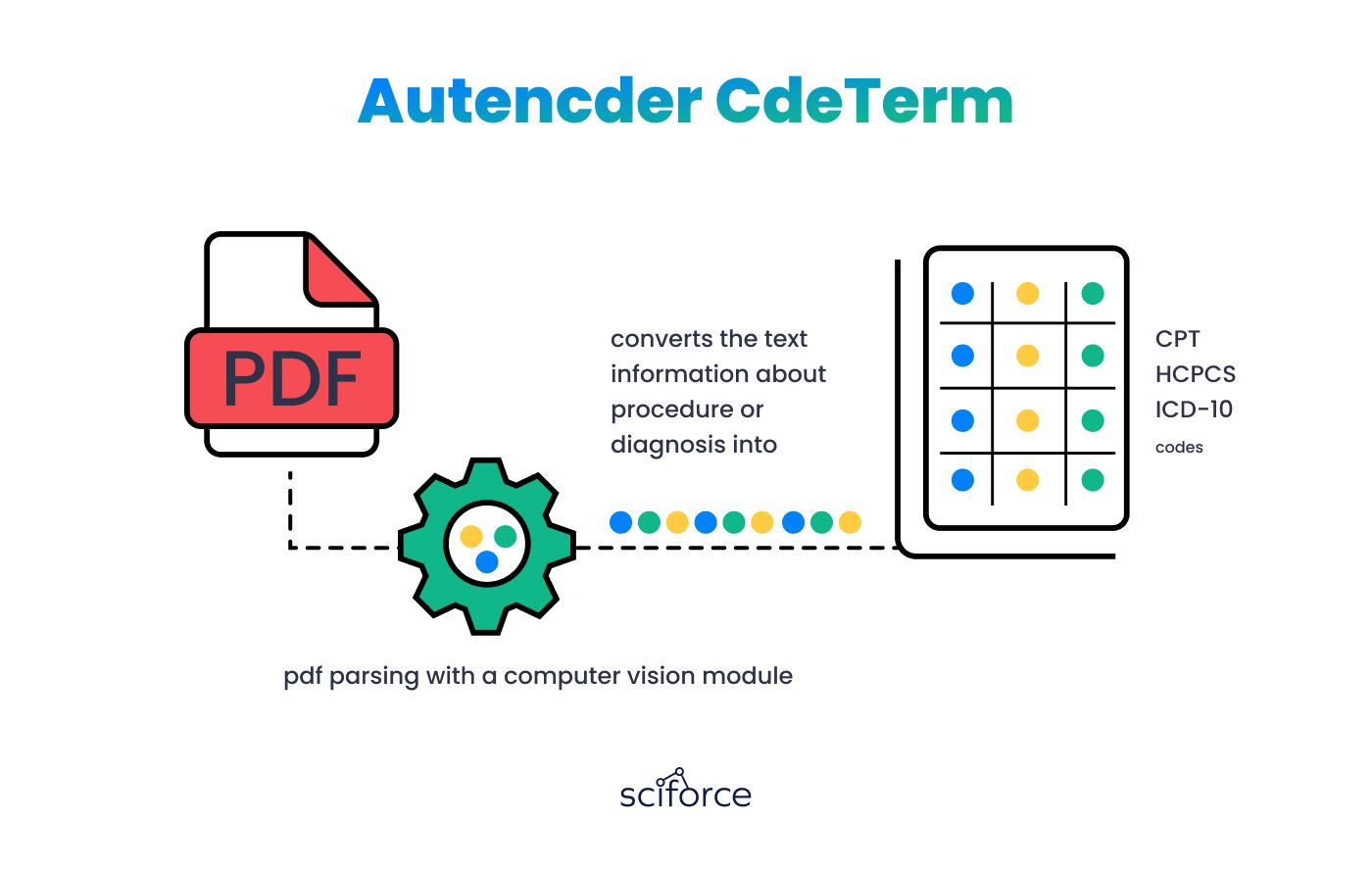
CodeTerm in this context is a neural network designed for processing and transforming complex data. It serves as the core of our AI model, functioning in three key areas:
PDF Parsing Module
This module converts unstructured data from PDFs into structured text using advanced PDF parsing techniques, efficiently organizing raw data for further analysis and processing.
Computer Vision Module
Utilizes computer vision technology to enhance data extraction and structuring from PDFs, increasing accuracy through visual recognition.
Free Text Coder
Processes structured data to identify healthcare-specific codes like CPT, HCPCS, and ICD-10. It translates textual information, such as diagnoses and procedures, into standardized codes, aligning data with healthcare ontologies for accurate interpretation.
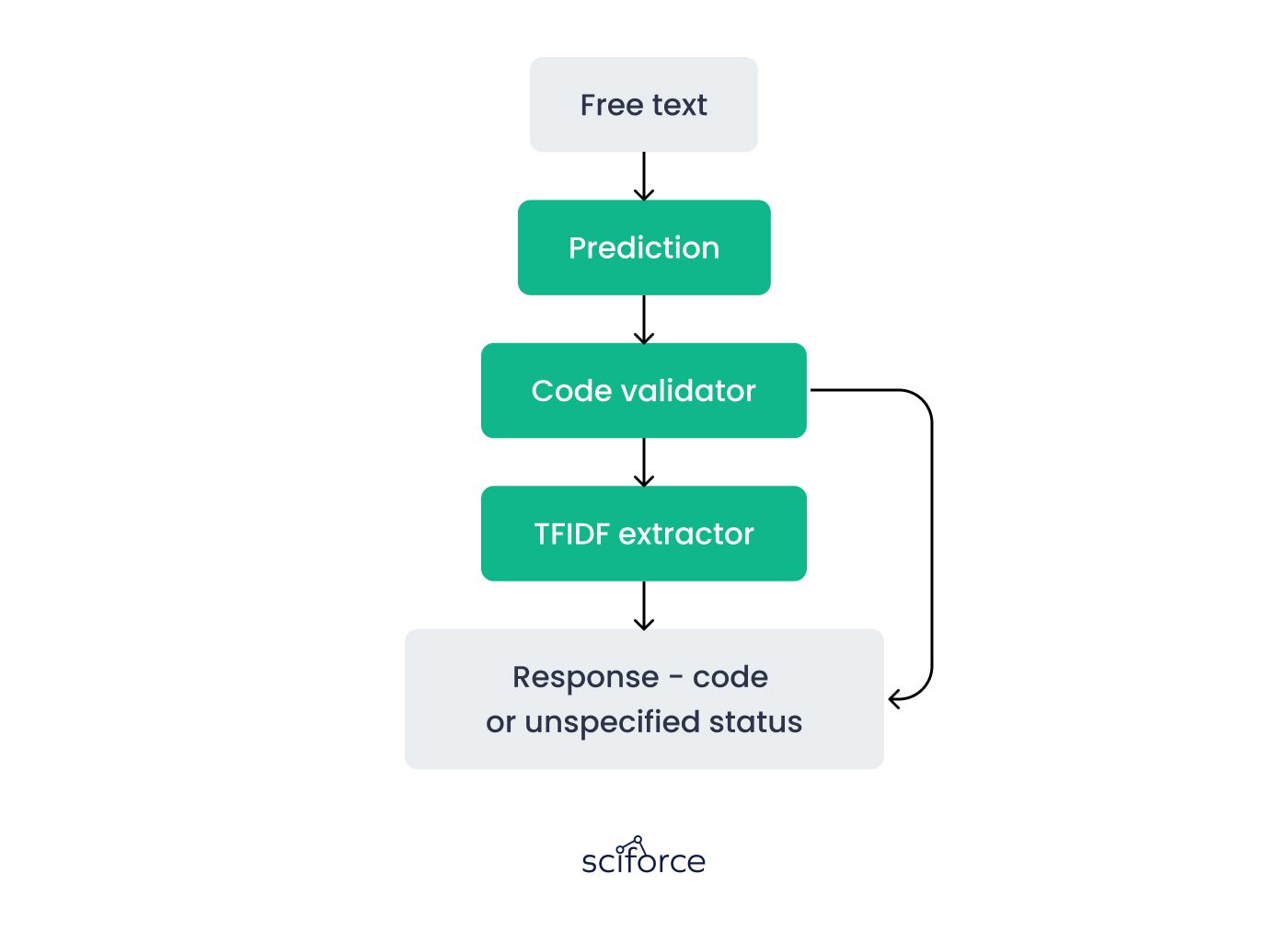
The CodeTerm component of our AI model follows a sophisticated workflow to process and analyze data, primarily from PDF documents. Here's how each step contributes to the overall functionality:
- NLP Parsing:
This step involves extracting text and identifying key terms from PDFs. It uses Natural Language Processing (NLP) techniques to discern relevant information, setting the stage for more detailed data analysis.
- Code Extraction and Validation:
Utilizing the Free Text Coder, this phase focuses on extracting specific healthcare codes from the parsed text and validating them for accuracy. This ensures that the data aligns with relevant healthcare coding standards.
- RegEx Extractor:
This tool applies regular expressions to extract coded data directly from the text. It's particularly useful for identifying and retrieving standardized codes embedded within the text.
Code Validator:
Following extraction, this step involves verifying the accuracy of the codes. The Code Validator cross-references each code against a comprehensive code dictionary, ensuring reliability and correctness.
- TFIDF Extractor:
To enhance the accuracy of code extraction, the TFIDF (Term Frequency-Inverse Document Frequency) Extractor analyzes text similarity, aiding in identifying the most relevant codes based on the context.
Computer Vision:
This step converts PDF documents into images and then applies image processing techniques to locate and identify keywords. It complements the text-based extraction methods by adding a layer of visual data analysis.
Merge Outputs:
Finally, the workflow concludes by merging the outputs from both NLP and Computer Vision processes. This integrated approach ensures a comprehensive and multi-dimensional analysis of the data, leading to more accurate and insightful results.
HealthClaim RejectionGuard
The HealthClaim RejectionGuard is a specialized component of our AI model, designed for precise prediction and analysis of insurance claim outcomes, particularly focusing on predicting the likelihood of claim denials:
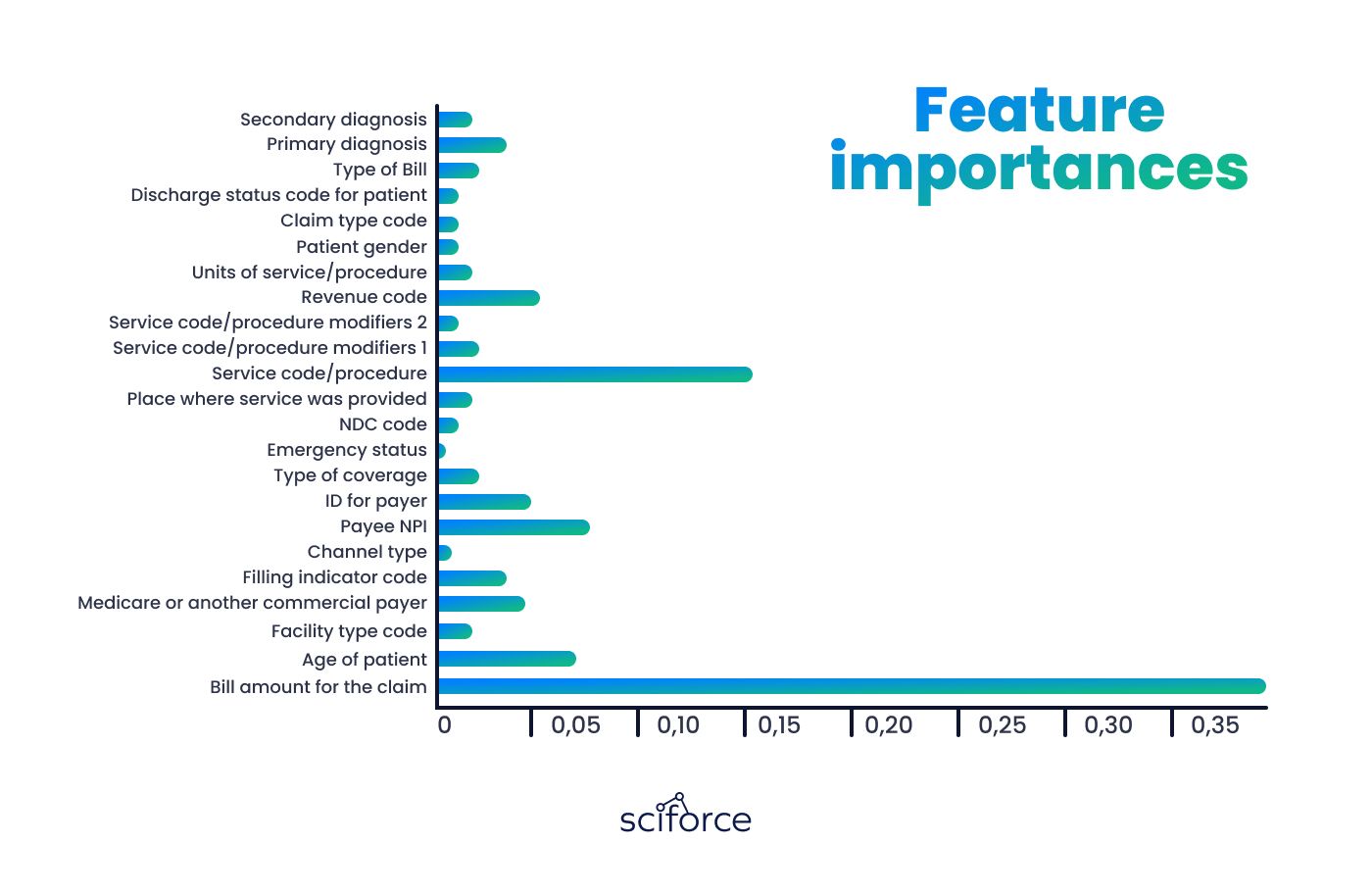
Data Preparation
In this phase, LabelEncoder is utilized to categorize various types of data, with a particular focus on the amounts paid for claims. This step is vital in preparing the data for accurate and effective analysis.
Data Processing
The dataset, consisting of over 7 million samples, is meticulously managed, with a division of 20% for testing and 80% for training purposes. This careful split ensures a balanced approach to training the model and evaluating its effectiveness on unseen data.
Model
At the heart of the HealthClaim RejectionGuard is the Random Forest algorithm, chosen for its robustness and accuracy in regression tasks. Key hyperparameters include n_estimators=10, max_depth=None, max_features='auto', and adjustments in min_samples_split as needed, allowing the model to learn from the data effectively.
Performance Evaluation
To assess the model's accuracy and reliability, we employ the Mean Squared Error (MSE) score. This metric provides a clear indication of the model's predictive performance, helping us fine-tune and enhance its capabilities continuously. Interacting with HealthClaim RejectionGuard and CodeTerm CodeTerm initially analyzes incoming claims, pinpointing missing billing codes. It then uses AI to transform text descriptions into structured, coded data, aligning them with healthcare coding standards. After CodeTerm processes the claims, the data, now well-structured, moves to HealthClaim RejectionGuard for in-depth predictive analysis.
HealthClaim RejectionGuard analyzes the data structured by CodeTerm, using machine learning models like Random Forest to predict whether the claim will be approved or rejected.
By launching this product, we've achieved significant results that positively impact both the healthcare industry and our clients:
Impact on industry
Our AI solution has significantly improved the way insurance claims are processed in the healthcare industry. It has successfully reduced the number of claim denials, making the entire management system more efficient. This change has not only cut down operational costs for healthcare institutions but also allowed for better use of resources. As a result, there's been a noticeable improvement in both the efficiency of operations and the quality of patient care across the sector.
Impact on client \ end-user
For our clients, including hospitals and medical practices, the benefits are significant. They've experienced fewer claim denials, leading to higher revenue and quicker reimbursements, thereby improving their financial health. Additionally, less manual processing means staff can dedicate more time to patient care, enhancing overall service quality.
Our goal was to lower the losses from denied claims and make the claim process easier, allowing healthcare staff to focus on patient care, not paperwork. Take a look at our case study to learn all about our solution.