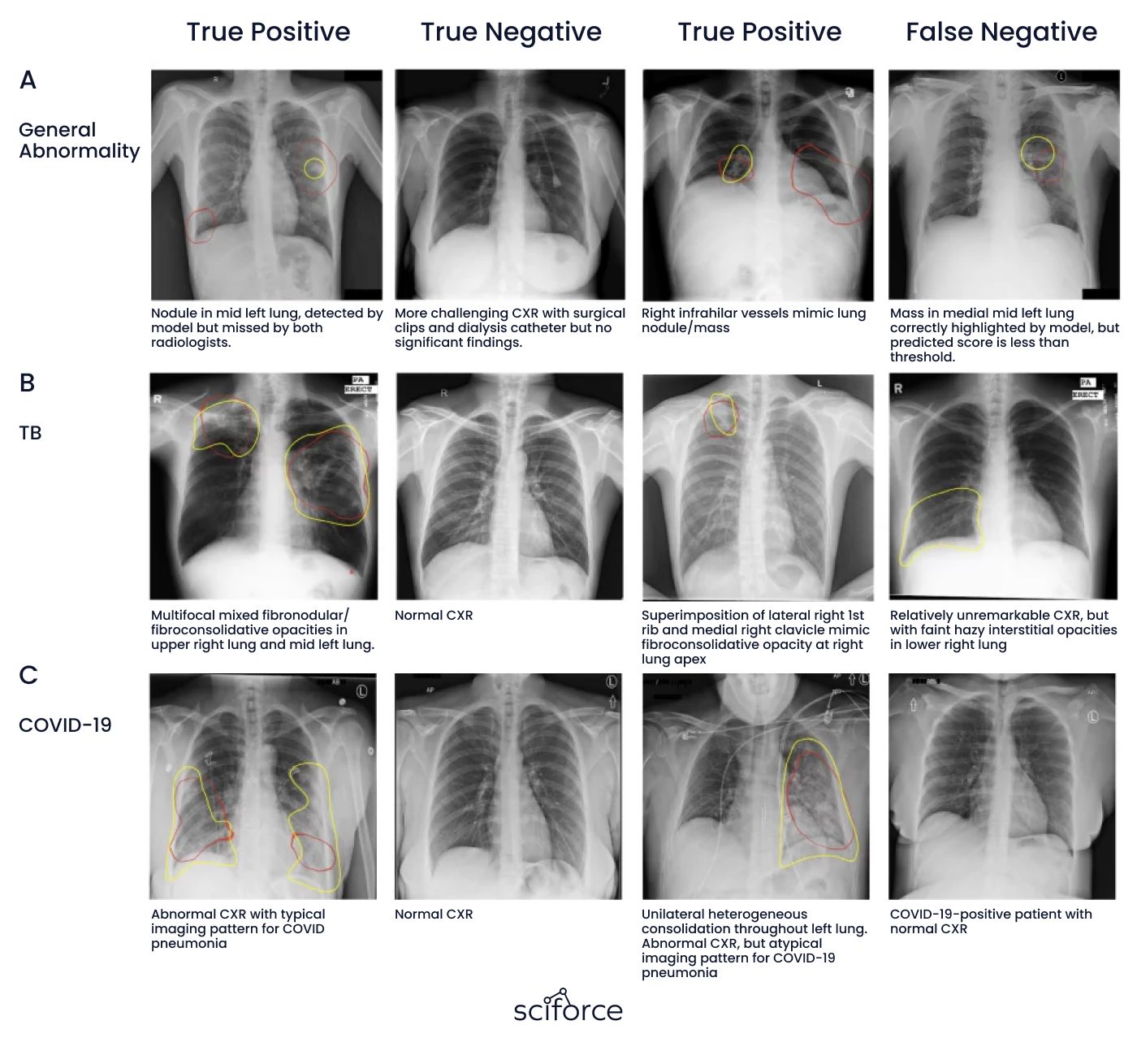
The imaging process significantly impacts the understanding of the disease progression and helps to administer effective treatment much faster. However, most general-purpose algorithms detect any abnormality that CXRs contain. That's why it is challenging to develop a classifier, as there are lots of abnormal findings on CXRs.
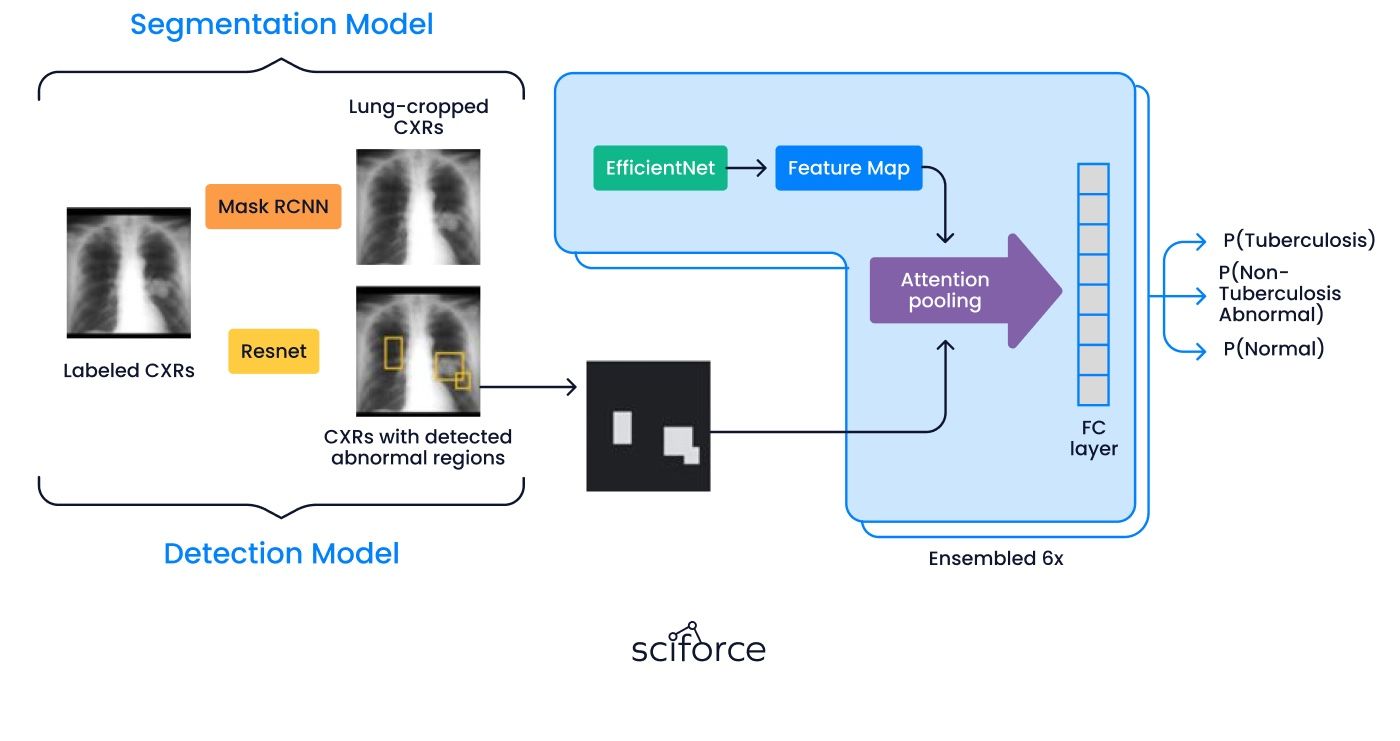
Meanwhile, we developed a DL model that precisely detects general abnormalities, unseen instances of tuberculosis, and COVID-19. The idea was to use computer vision, statistical and machine learning algorithms.
Inconsistent Results in CXR Analysis:
The quality of imaging can be affected by various factors, such as equipment standards, medical expertise, and time constraints, leading to inconsistencies in the results.
Over-Detection by General Algorithms:
High false positives increase the workload for medical staff.
Avoiding Overfitting and Ensuring Model Generalization:
It was crucial to prevent the model from overfitting to a single dataset and to ensure its ability to generalize to new data and populations. This required careful selection of validation methods, cross-validation, and testing on independent datasets.
Integration of Multiple Technologies and Approaches:
Combining computer vision, statistical methods, and machine learning algorithms required coordination among different technological approaches. This necessitated synchronization among multidisciplinary teams and experts to ensure a cohesive solution.
Detection of Specific and Previously Unseen Diseases (Tuberculosis, COVID-19):
Detecting specific diseases like tuberculosis and COVID-19, which may have atypical manifestations on chest X-rays, poses a significant challenge. The algorithm must be sensitive to various pathologies, including those not previously encountered.
Optimizing for Clinical Relevance:
Aligning the model with real-world medical practices required input and validation from clinical experts to ensure its diagnostic accuracy and relevance.
Incorporating Feedback from Medical Experts to Improve the System:
Ensuring the AI model’s diagnostic accuracy and clinical relevance requires continuous input and validation from medical experts. Integrating this feedback presents challenges such as coordinating with clinicians' busy schedules, translating complex medical insights into technical adjustments, and iteratively refining the model to align with real-world medical practices.
Data Standardization Across Diverse Datasets:
The solution needed to function accurately across different datasets, each with unique characteristics and standards, posing a challenge for standardization and reliable generalization.
Ensuring Patient Privacy and Data De-identification:
Using de-identified datasets for training and testing the model necessitated adherence to ethical standards and ensuring patient confidentiality. This added complexity in data handling and required implementing additional security measures.
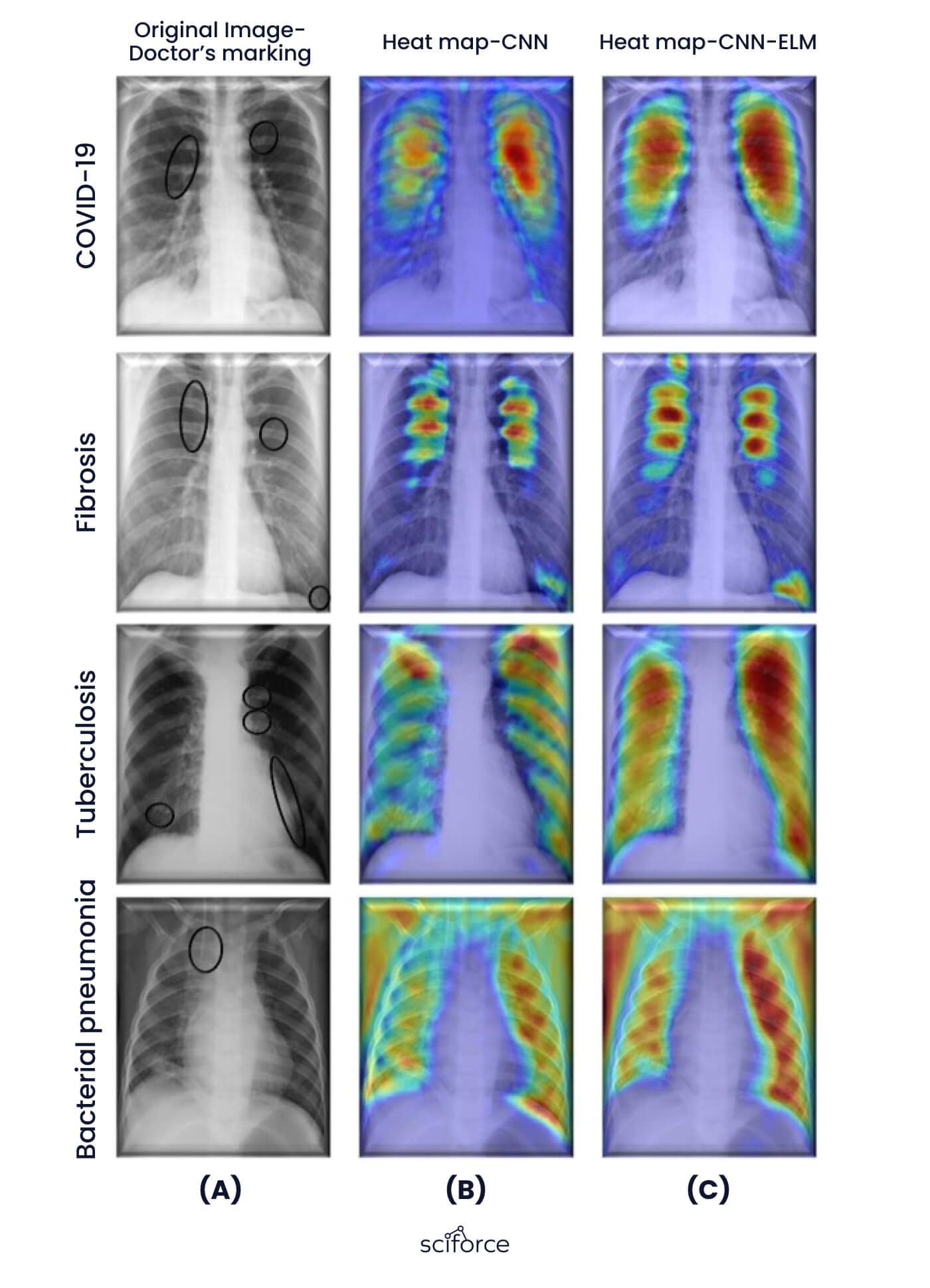
To ensure accurate detection of lung pathologies in chest X-rays, we used a deep learning model based on the EfficientNet-B7 architecture. This model is highly accurate and well-suited for detecting abnormalities like tuberculosis and COVID-19. It is also robust enough to work across different datasets and integrate smoothly into existing diagnostic workflows.
Why EfficientNet-B7?
Alternatives Considered
We initially explored simpler machine learning models and traditional computer vision methods. However, these approaches couldn’t meet the accuracy required for detecting rare or complex abnormalities. For example, they struggled to identify nuanced signs of tuberculosis and COVID-19. This led us to choose a more advanced deep learning solution.
By adopting EfficientNet-B7, we created a reliable and precise tool that meets the demands of healthcare professionals while ensuring compatibility with their workflows.
Accurate Detection of Lung Pathologies
The system uses AI powered by the EfficientNet-B7 model to detect a wide range of lung issues in chest X-rays, including hard-to-spot conditions like tuberculosis and COVID-19, ensuring high accuracy.
Automated Prioritization of Critical Cases
The system prioritizes abnormal cases, moving them to the top of the review queue so doctors can focus on the most urgent patients first, speeding up care.
Minimized False Positives
The model is designed to identify only meaningful abnormalities, reducing false positives and unnecessary work for medical staff.
Customized AI Model
The deep learning model is specifically built to handle different types of chest X-ray images, ensuring accurate detection of both common and rare lung conditions.
Trained on Diverse Datasets
The system was trained and tested using multiple datasets, including public ones like ChestX-ray14 and client-provided data, to ensure it works well across different patient groups and imaging systems.
Standardized Data Handling
Data preprocessing ensures the system can adapt to new datasets, avoiding overfitting and maintaining consistent performance.
Fast and Scalable
The system can process large numbers of chest X-rays quickly, making it suitable for busy hospitals and diagnostic labs.
Expert-Driven Data Labeling
Medical professionals labeled the training data, ensuring the system learned from high-quality, accurate examples.
Continuous Updates with Expert Feedback
Regular input from radiologists and pulmonologists helps improve the system, keeping it relevant and effective in real-world use.
Fits into Existing Workflows
The system integrates smoothly into hospital diagnostic processes, reducing the workload for doctors and speeding up results.
Patient Privacy and Security
The system uses de-identified data to protect patient information, complying with strict privacy rules and ethical standards.
Clear Reporting and Documentation
The system provides detailed reports that highlight detected issues and their urgency, helping doctors make informed decisions. It also comes with technical documentation to support easy setup and long-term use.
NLP for Better Image Annotation
Natural Language Processing (NLP) techniques were used to analyze medical reports, improving how the system labels and understands the data.
Building the chest X-ray analysis system required addressing challenges like varying image quality, diverse patient data, and clinical workflow needs. From handling diverse datasets to ensuring clinical relevance, we focused on building a system that addressed real-world diagnostic needs.
Our team tested the prioritization feature in real-world scenarios, demonstrating its ability to streamline case reviews and improve response times. To address varying image quality, we applied advanced preprocessing and validated results with medical experts. To ensure that the model performed well with new data, we minimized overfitting by training on diverse, de-identified datasets.
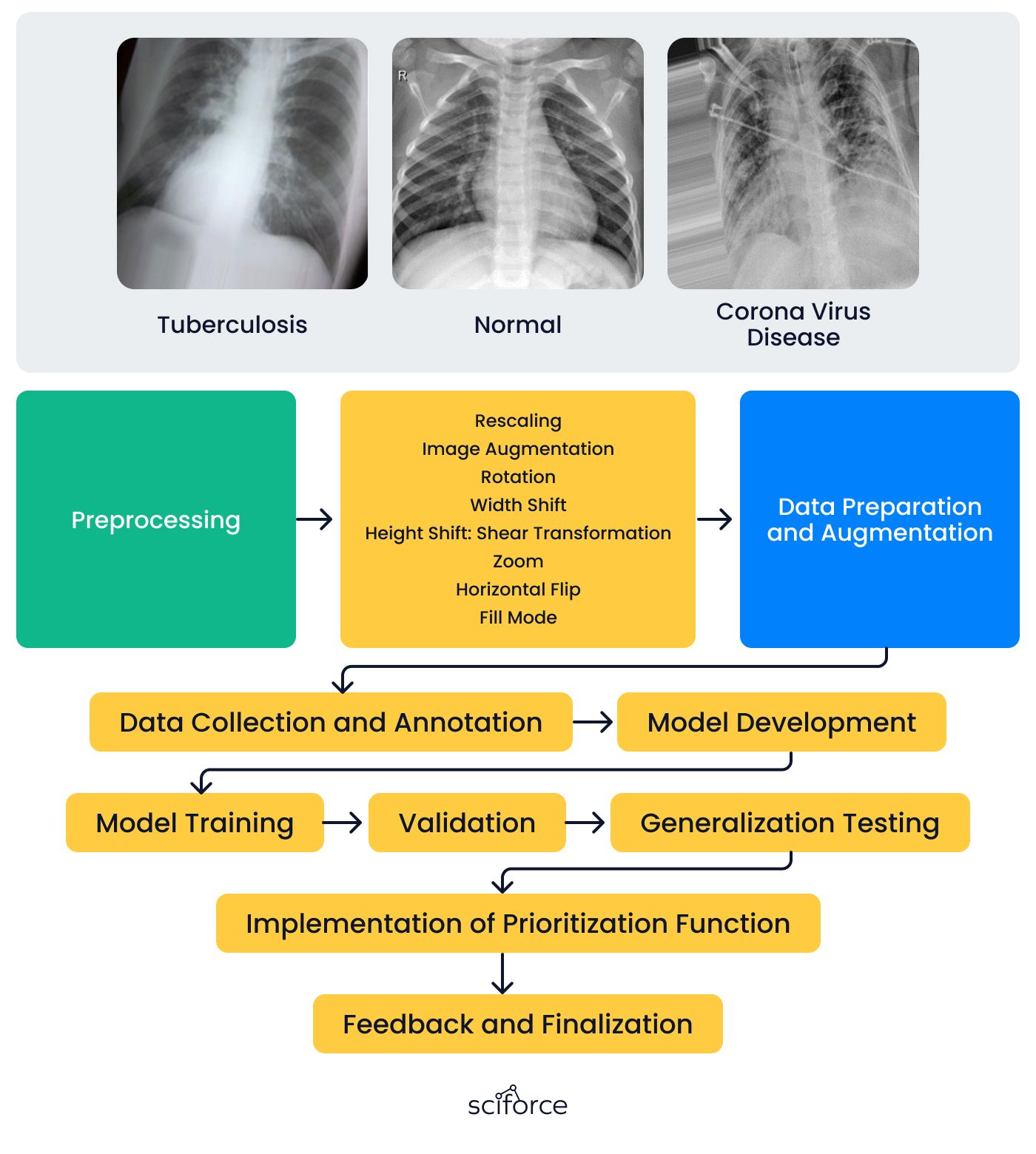
1. Data Collection and Annotation
We collected chest X-ray datasets from client-provided medical records and public sources like ChestX-ray14. Radiologists carefully labeled the images, identifying conditions such as tuberculosis, COVID-19, and other abnormalities.
2. Model Development
We chose EfficientNet-B7 for its strong feature extraction capabilities and ability to handle image quality variations. Configuring it as the backbone of a detection system for lung pathologies like tuberculosis and COVID-19, we fine-tuned it with additional layers to enhance sensitivity and reduce false positives.
3. Model Training
The team trained the model on labeled datasets, including tuberculosis and COVID-19 cases, to recognize subtle patterns in chest X-rays. Data augmentation enhanced its reliability across diverse imaging conditions, ensuring accurate identification of abnormalities.
4. Validation
Radiologists and pulmonologists carefully reviewed the model’s predictions to ensure it could accurately identify lung issues like tuberculosis and COVID-19. They provided feedback on areas needing improvement, such as detecting subtle abnormalities and reducing false positives.
5. Generalization Testing
Testing included diverse datasets, such as ChestX-ray14 and client-provided data, to evaluate performance across various patient groups and imaging systems. Preprocessing techniques, including normalization and standardization, addressed differences in image quality and equipment.
The system includes a prioritization feature that flags and ranks abnormal chest X-rays, ensuring critical cases appear first for faster attention. Simulations in real-world settings demonstrated its effectiveness in improving review efficiency and speeding up responses for urgent cases.
7. Feedback and Finalization
Radiologists and pulmonologists gave regular feedback to improve the system’s accuracy, focusing on detecting subtle abnormalities and reducing false positives. This input led to updates in the model and prioritization feature. Final adjustments ensured the system worked smoothly with existing clinical workflows, making it easy to use and effective in real-world healthcare settings.
- Better Diagnostic Accuracy
The system detects lung issues like tuberculosis and COVID-19 with over 95% precision, reducing errors and improving diagnosis quality. Accuracy rates have increased by 15-20% compared to manual methods, ensuring fewer missed cases.
- Faster Diagnosis
Automated prioritization has reduced the average time to review critical cases by 30-40%, allowing faster response and treatment. Patients now receive diagnoses within minutes instead of hours in urgent scenarios, leading to better outcomes.
- Less Workload for Medical Staff
By automating routine tasks, the system saves medical staff up to 3-5 hours per day, enabling them to focus on complex cases. Workflows have improved efficiency, with a 25% reduction in time spent on manual image reviews.
- Adaptable to Different Settings
The system maintains consistent accuracy of over 90% across diverse datasets, including variations in imaging quality and patient demographics. This makes it suitable for use in both high-resource hospitals and smaller clinics.
- Improved Patient Care
Faster and more accurate detection of diseases means patients receive timely diagnoses. This has resulted in a 20% reduction in late-stage disease detections, improving overall health outcomes.
- Stronger Market Position
The AI solution has been adopted by 10+ healthcare institutions within the first six months of deployment, helping the client strengthen their market presence. Partnerships with leading healthcare providers are expanding the client’s reach.
- Cost Savings
The system has reduced operational costs by an estimated 20% per patient, enabling healthcare providers to process more cases at a lower cost. Efficiency improvements have also cut diagnostic overheads by 15-30%.
- Building Trust Through Compliance
The use of de-identified data and adherence to privacy standards has resulted in 100% compliance with GDPR and HIPAA regulations. Feedback shows a 90% satisfaction rate among healthcare professionals using the system.